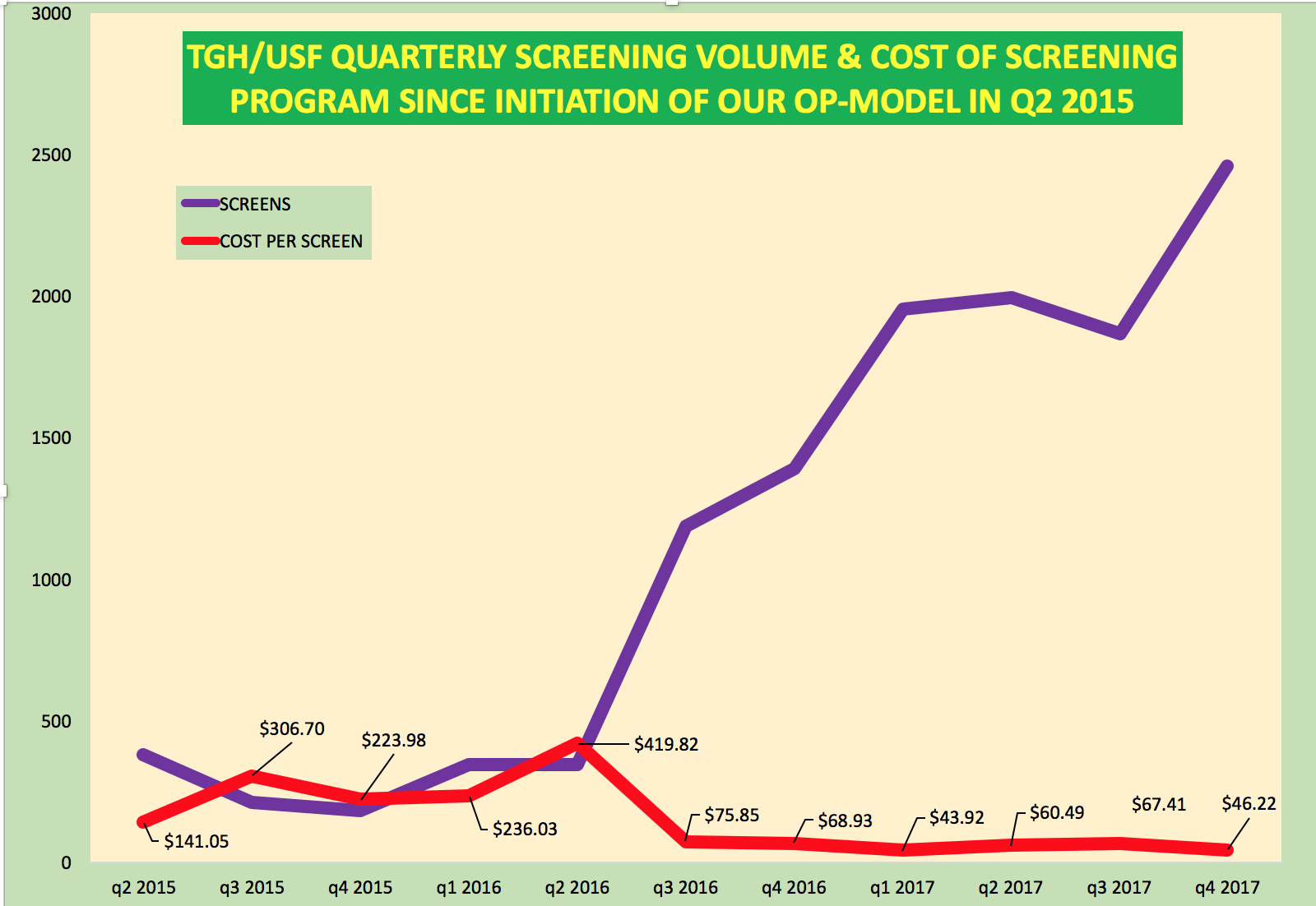
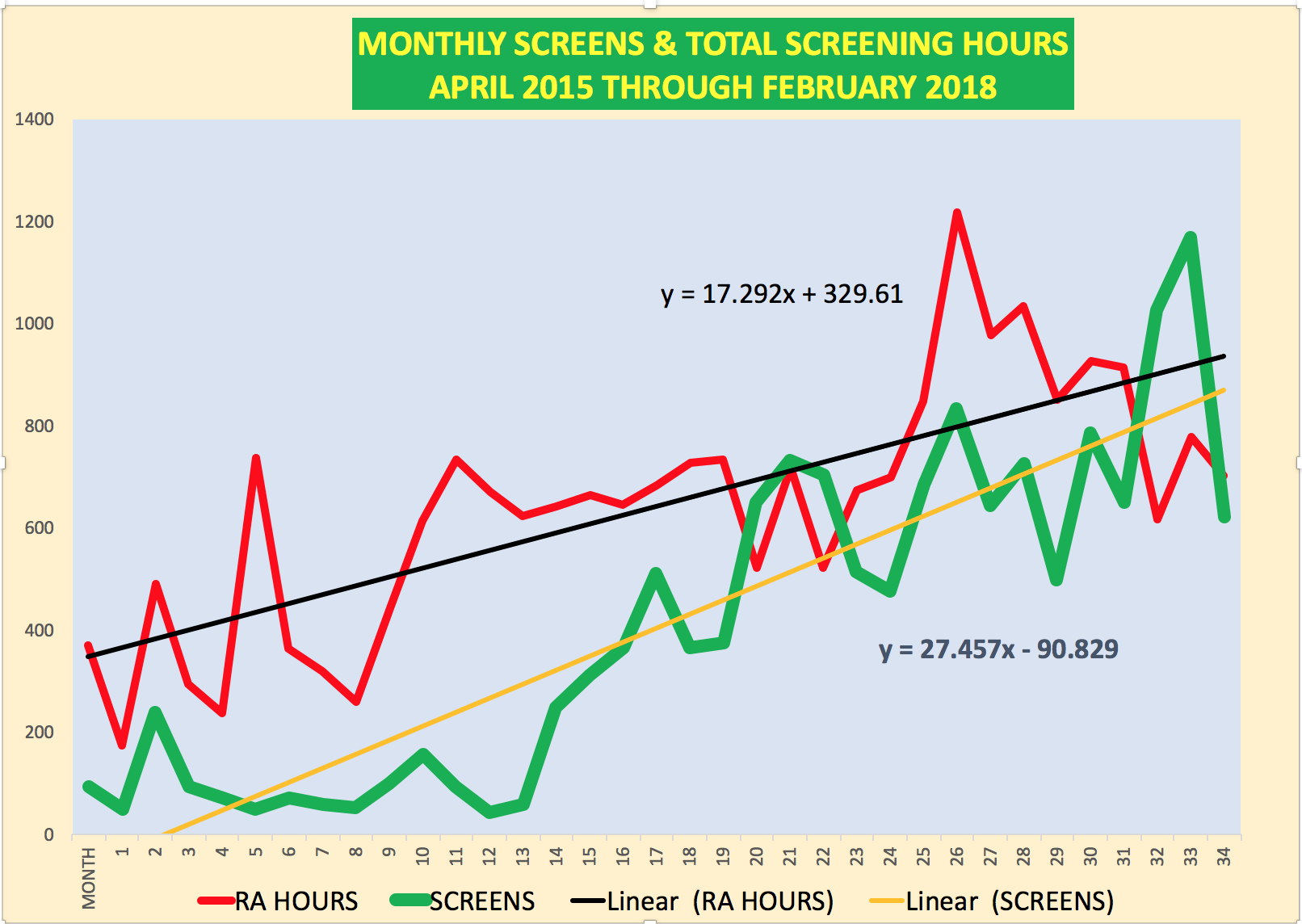
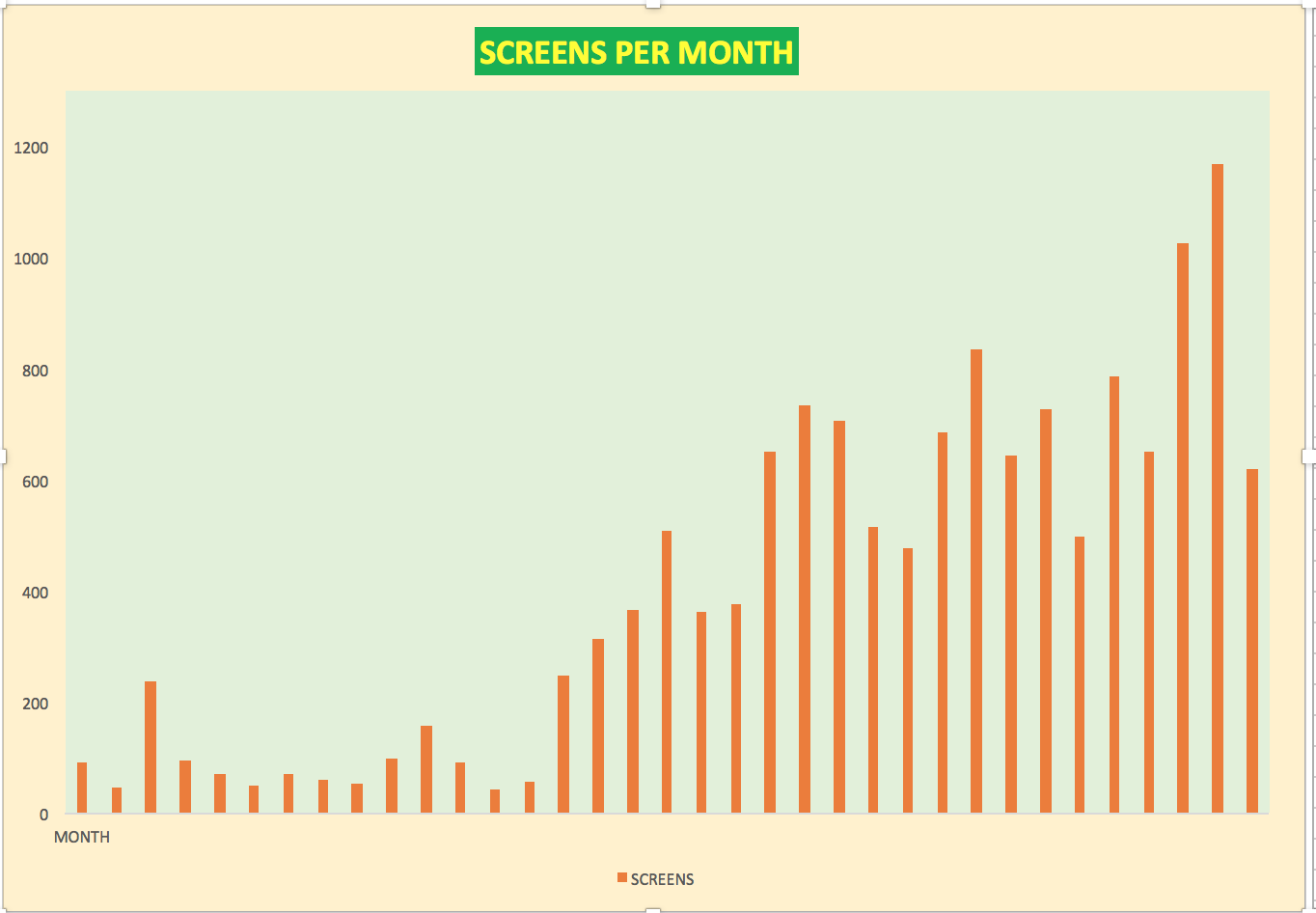
The TGH/USF ED Based Acute Care Research team increased our efficiency since initiating a novel operational model in Q2 2015 to enroll patients and conduct research that is synergistic to overall TGH goals while also integrating scholarly opportunities across learner types (residents, medical students, ARNP students, and premedical students) and across disciplines.
DISCLAIMER:I am working out my thoughts for an ACEP SA 2018 paper on how we designed and implemented an acute care research program based in the emergency department
10 KEY ELEMENTS TO THE SUCCESS OF THE TGH/USF ACUTE CARE RESEARCH PROGRAM
- vision that a research program can operate like any other service line with an emphasis on high quality care delivery when the patient comes to us (2am on a weekend), not when we might desire a patient to present (9-5 on weekdays)
- a mission for acute care research to operate like any other acute care service line with the ability to provide a drug, a device or a procedure 24/7 with appropriate staffing, infrastructure and buy in place
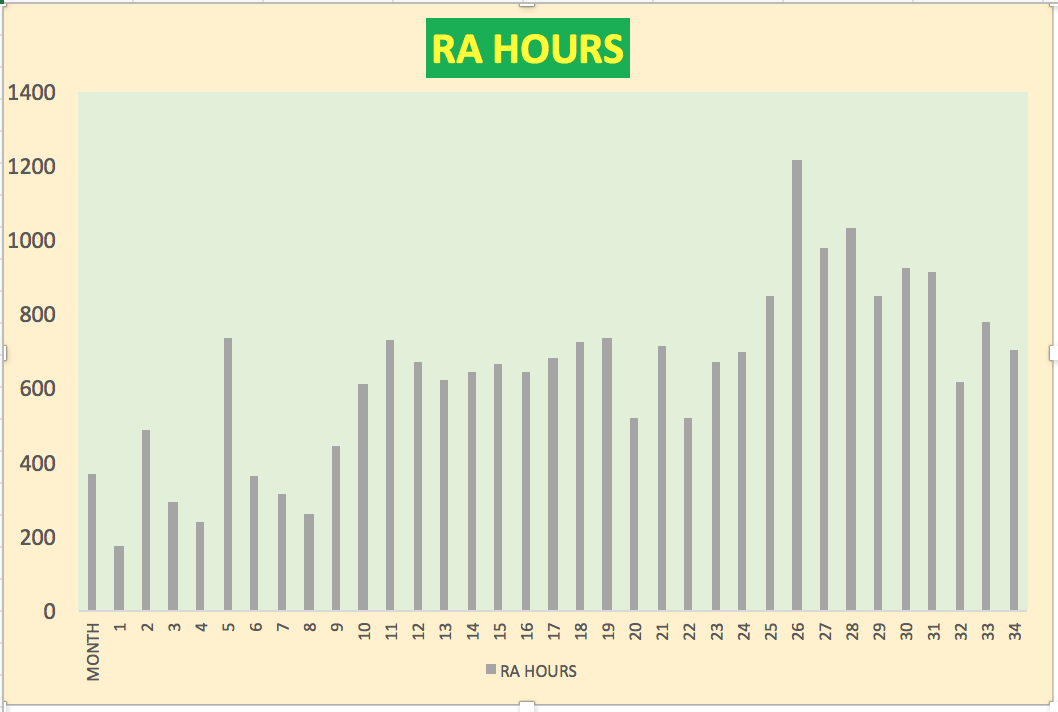
- utilization of cross covering shift workers based on an emergency medicine model of care delivery (paid research assistants, research nurses)
- maximization of electronic medical record potential for ROI through optimization of clinical alert processes to screen the entire patient population for inclusion/exclusion criteria and to alert both clinically active providers that a potential research patient may be present during an acute encounter
- lean based approach that considers the PI as customer with an emphasis on our ability to make a PIs study achieve success as well as a streamlined flow for providers and staff to contact the research team (RESEARCH HOTLINE: 813.394.3025) and a faster turnaround time from study idea to initiation via a slimmed down feasibility process after IRB
- leverage of revenue (PI fees) to create a budget for formal premedical course work, paid course assistant positions, and small seed funding for investigator initiated studies
- formal funding of social science PhD students to expand scope of research questions while providing educational and research opportunities to additional learners
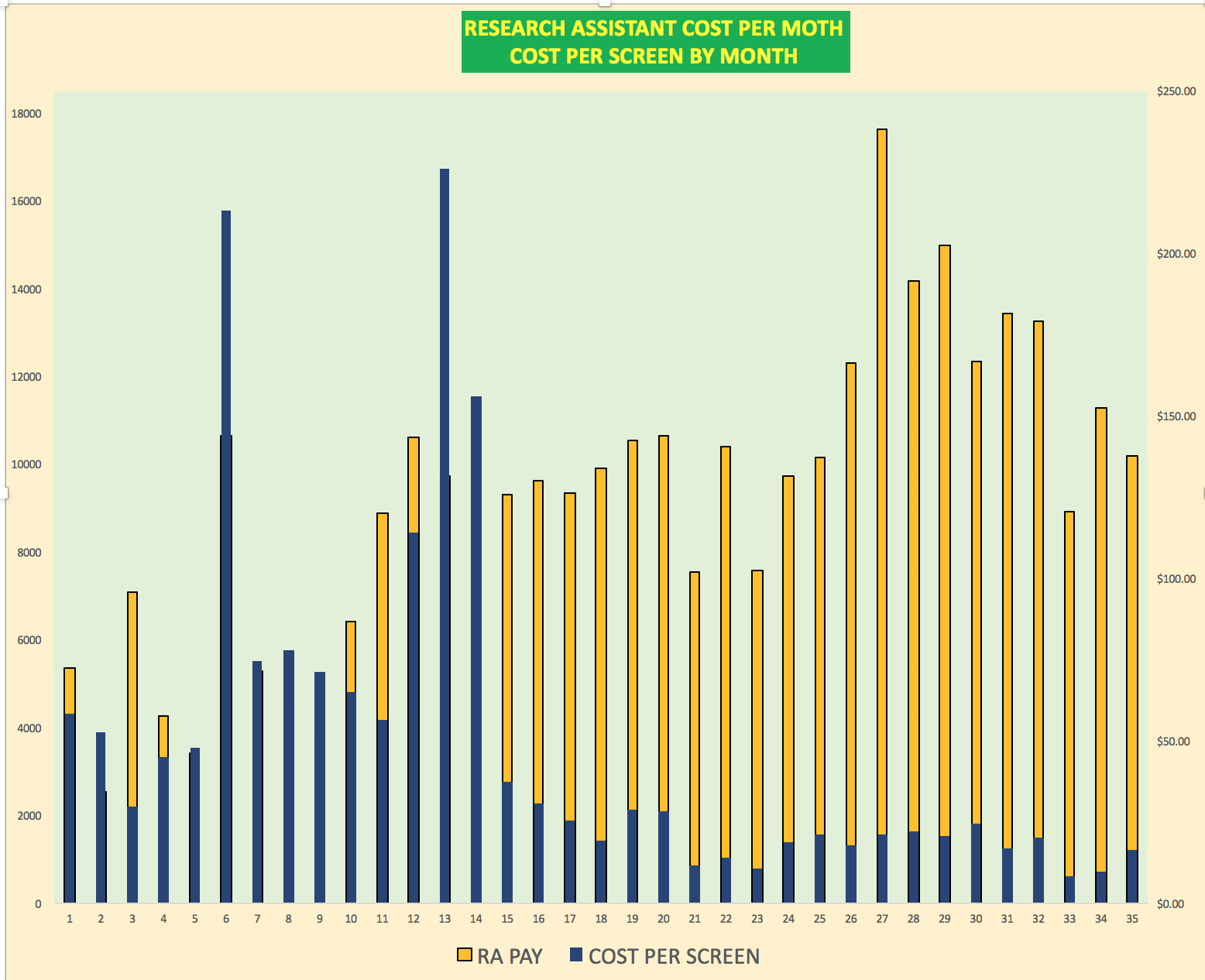
- clear negotiation with research sponsors that our work flow includes paid research assistant 24/7 and RN coverage 24/7 and those activities must be funded in study budget as we will not compromise our quality and track record of success
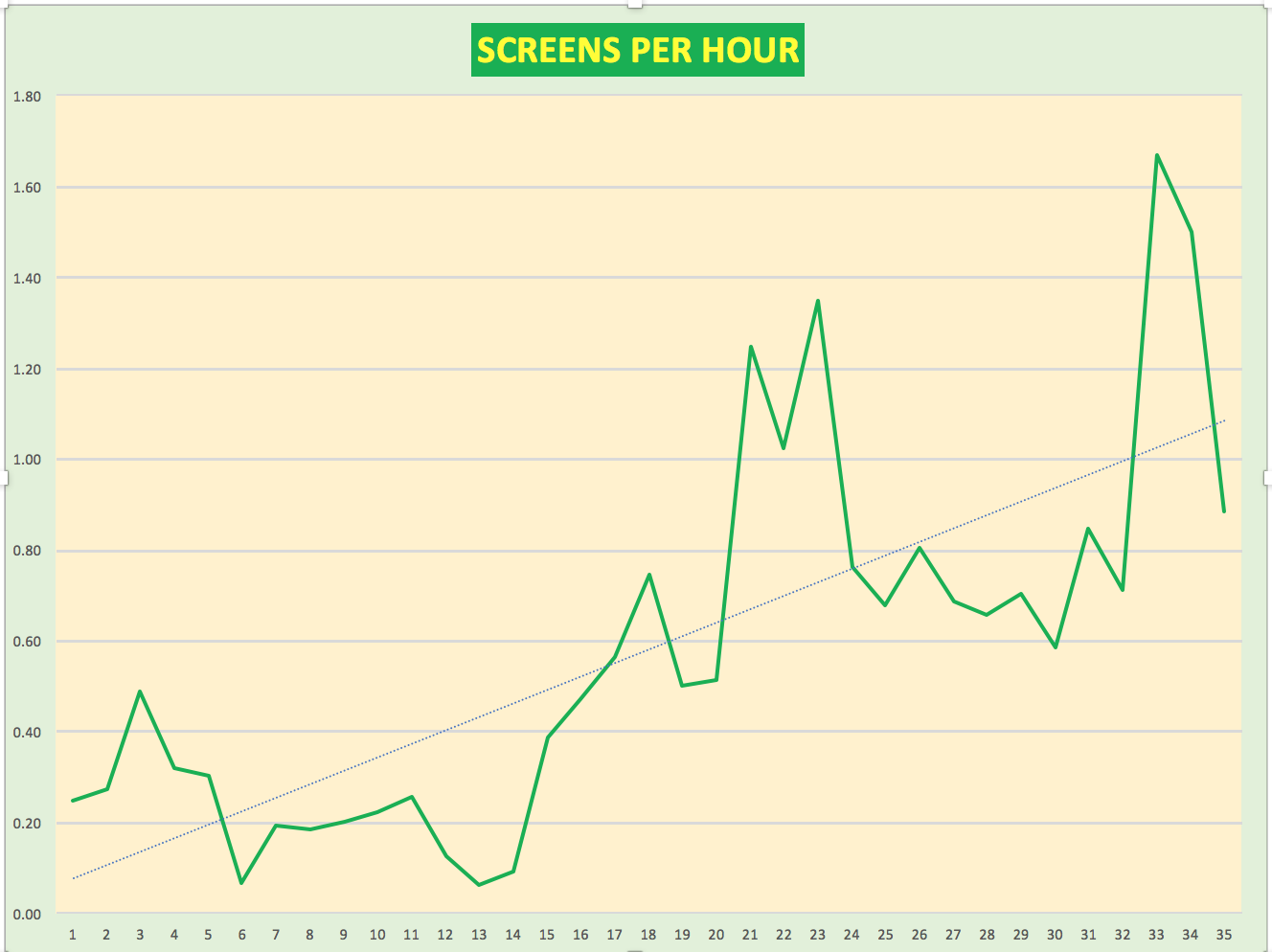
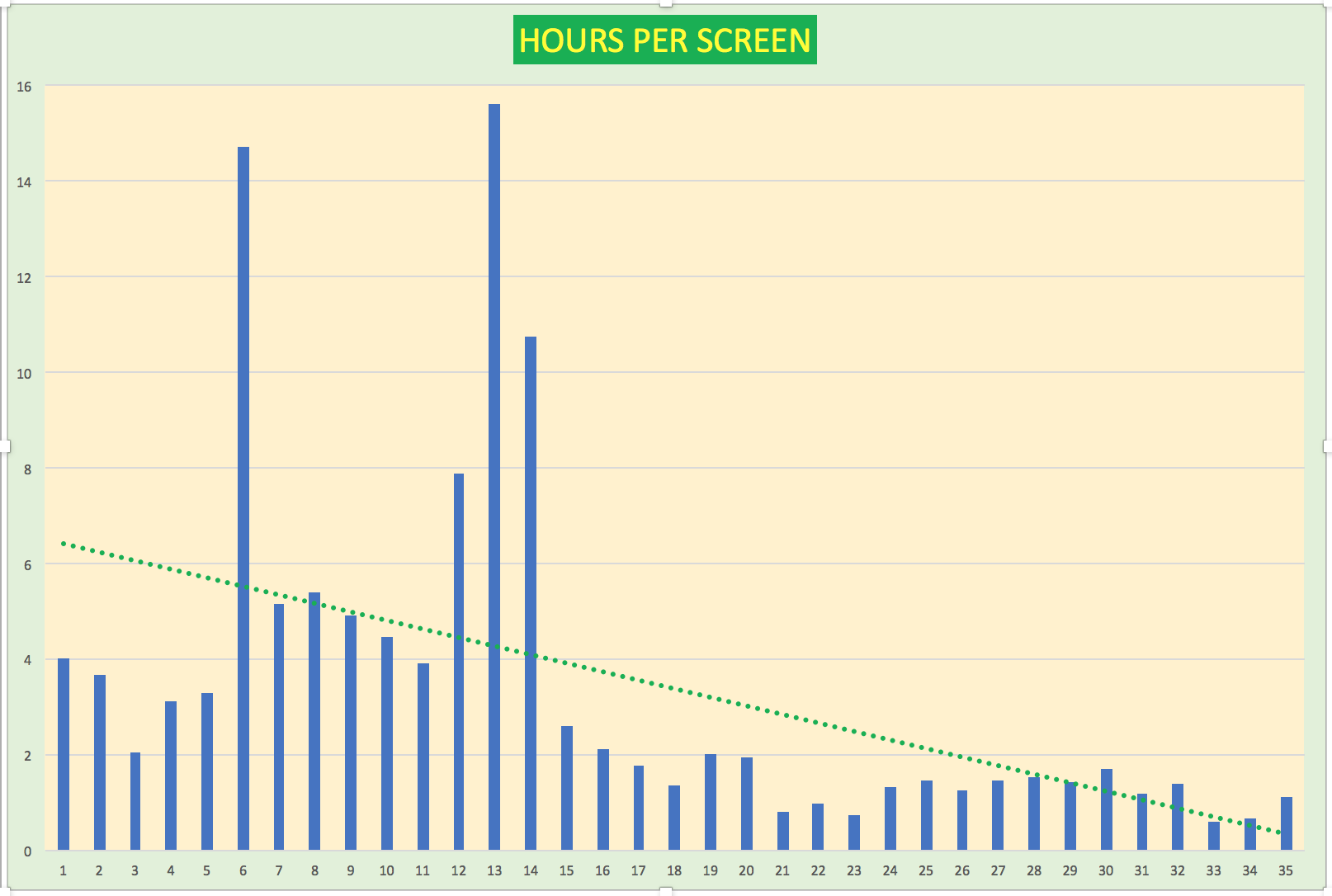
- development of research throughput and quality metrics that allow internal team members to meet expectations and for external stakeholders to realize our value
- continued efforts to deliver transparent pricing and cost understanding to our PIs and sponsors
ok – so what made us more efficient? i will talk about that on the next post but in the meantime, please add comments below – especially if you are or were a member of the team!